Investigations, Investigations, Investigations (Part 4)
Image courtesy of [anankkml] / FreeDigitalPhotos.net
However, when diagnoses are unclear or can't be differentiated, that's where investigations come in. Sadly, today they're often over-used, but when used appropriately they offer a wealth of information that can help tailor all important management and get the patient on the path to recovery faster.
Following on from part one, where we looked at urine, part two which look at bloods, and part three which looked at imaging, this multi-part post will take a look at some of the common investigations performed, what they can tell us and the reasons why and when they should be used.
Our fourth and final part deals with some other tests that didn't fit into the above categories, but which are as important in assessing patients and helping to reach a diagnosis.
Part Four- Everything Else!
ECG/ 24hr tape/ exercise ECG
An ECG (or EKG, electrocardiogram) looks at the electrical activity in the heart. While heart muscle beats on its own, it needs nerve activity to set things like rate (how fast it's beating) and contractility (how hard it beats). ECGs are actually extremely useful and can give a lot of information outside of just seeing the heart rhythm. We can do standard 12-lead ECGs, giving us an indication of what the heart is doing now, or 24hr tapes, where a holter is worn for 24hrs and the heart rate recorded continuously. This is often good to pick up abnormal heart rates associated with palpitations.
It's mostly used to detect arrhythmias (abnormal heart beats, such as atrial fibrillation (irregular pulse), supraventricular tachycardias (too fast), heart block and bradycardias (too slow), and 'missed' beats), but it can also look for cardiac disease (ischaemic heart disease or full blown myocardial infarction [heart attack], heart infections (pericarditis), heart enlargement, and in the case of heart failure it can even give us prognosis (how severe the heart failure is and the outcome of this). It can also pick up problems with the lungs, such as in pulmonary embolism, which can cause strain on the right chambers of the heart.
However, having a normal ECG doesn't rule out there's a problem with the heart, so it's not got a very good negative predictive value. Nevertheless it's an extremely useful tool in practice.
Further reading:
1. http://www.patient.co.uk/health/electrocardiogram-ecg
2. http://www.bhf.org.uk/heart-health/tests/ecg.aspx
24hr BP monitoring
Whenever we visit the doctors for a blood pressure check, it's always high, right? But how can we tell it's because of 'whitecoat hypertension' (the BP goes up because you're stressed about seeing a doctor), or actual 'essential hypertension'? We measure BP over 24 hours, of course. This has become the standard for diagnosing true hypertension and helps to plan what treatments to start on.
The patient is given the machine to take home, and the monitor takes several readings through the day and night. If the overall average value and night values are above the limit, then we can start treatment. Not only is this test more accurate than measuring BP at single points on different days, it saves on the patient having to keep returning to have BP checks for diagnosis.
Some problems with this test though are that some patients can't tolerate it, and the fact that the machine needs to be loaned out. It also needs a patient to be aware of how to use it (so for example it could be difficult to perform in a frail elderly person requiring a lot of care).
1. http://www.bloodpressureuk.org/BloodPressureandyou/Medicaltests/24-hourtest
Pulse dopplers and ABPI
A doppler machine works on a similar principle to ultrasound, except instead of projecting images, it projects sound. This can be very useful in looking at blood flow through arteries, as blood makes sound as it flows. We can measure this while changing blood flow as well via a blood pressure cuff, and hence we can give a ratio of how good the circulation is at the hands and feet. This is known as an 'ankle brachial pressure index', where we compare blood flow in the arm and leg at a given pressure. The lower this number is, the more likely it is you have severe circulation problems in the leg, which can lead to complications.
It's also used a lot in pregnancy, as we can detect the fetal heartbeat from around 14-16 weeks onwards, and is useful to check fetal wellbeing if the mother is experiencing problems.
However, the problem with this test are that it can give false readings (as patients with diabetes might have normal ABPIs but still have poor circulation), and it needs special training to be performed.
Further reading:
1. http://www.webmd.com/dvt/doppler-ultrasound
2. http://www.westcoastvascular.com.au/services/doppler-test/
Nerve conduction studies
We also have the means to measure how well nerves transmit sensation and information! These are called nerve conduction studies and are very specialised. We measure the current running through a specific nerve (such as the median nerve in the wrist), and the speed and amplitude tells us whether there is any nerve damage. We can also do this following trauma or fracture and the patient still complains of nerve symptoms (tingling/ pins and needles/ numbness) following resolution of the original injury.
This test is necessary for a confirmation of a diagnosis of carpal tunnel syndrome before any surgery is planned. This is to also have documentation of nerve function pre-surgery, so that we know if the damage was there before anything was done.
The drawbacks are that it can be an unpleasant procedure (as needles are used to look at nerve function in specific muscles when testing for motor problems), it's very time consuming, and it needs specially trained neurophysiologists to perform.
Further reading:
1. http://www.patient.co.uk/health/nerve-conduction-studies
2. http://drprafullkdavemd.com/ncs.php
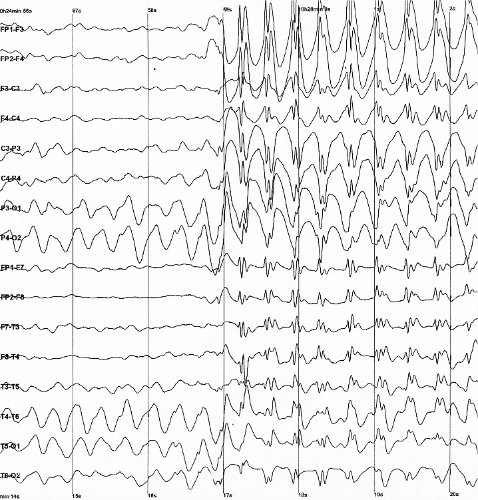
Electroenecephalogram (EEG)
Electroencephalograms are similar in principle to the ECG/EKG, except these look at the electrial activity in the brain. This is often done to look for epilepsy. They can also be co-ordinated with video to look at what the EEG does if the patient has a seizure. However, they can be very difficult to interpret, and like with ECGs, having a normal EEG doesn't mean there's nothing wrong. Yet as with most tests, it needs to be interpretted in the clinical context to be of diagnostic value.
Further reading:
1. http://www.nhs.uk/Conditions/EEG/Pages/Introduction.aspx
Spirometry
This is a breathing test that looks at the capacity and function of the lungs. It can be used to diagnose a variety of lung diseases such as asthma, COPD, and fibrotic lung disease. It's also good as a monitoring test to see if there is improvement/ worsening of lung function over time and before/ after a course of treatment. The patient is told to breath into a tube which measures air flow. By taking big breaths and breathing out quickly, we can then get measurements of lung capacity and volume, normal breathing volume, and how fast the patient can expel air from their lungs.
However it's a very time consuming test and does rely on accurate patient performance. It's also difficult to do in young children, as they might not understand instructions.
Further reading:
1. http://www.patient.co.uk/health/spirometry-leaflet
Angiography/ colonscopy/ arthroscopy
These can be both diagnostic and therapeutic tests, meaning that it can diagnose a problem and treat it at the same time. We'll take them individually.
Angiography looks at the blood vessels, typically of the heart, but they can look at any artery (the picture above shows the arteries of the brain). For the former, a catheter is placed in an artery at the wrist or groin, and dye injected. X-ray images are then taken at the same time, giving us a live 'snapshot' of blood flow through the coronary arteries. If there is any obstruction, from a plaque for example, then a stent can also be placed to remove the obstruction and improve cardiac blood flow, lessening symptoms of chest pain/ angina etc. The same principle is used for other vessels, such as looking in the limbs, again for obstruction or aneurysms.
Colonscopy is using a fibre-optic camera to have a direct look at the bowel. This is the same for any 'scopy' test- so arthroscopy is putting a camera into a joint such as the knee, nasendoscopy gives a direct look at the nasal airways/ throat, endoscopy looks at the oesophagus (food pipe) and stomach. If any abnormalities are seen, instruments can be inserted in the fibre-optic tube and biopsies (tissue samples) can be taken. In some cases treatment can be done as well, such as removing small polyps from the bowel, injecting stomach ulcers, or washing out/ trimming cartilage in joints.
The major drawback in these tests are that they are very invasive, and have small but significant complications and risks. They also need to be performed by specialists in hospital, and this might require overnight hospital stays. Also, anything needing extensive treatment, like joint replacement/ multiple blocked arteries/ multiple polyps in the bowel can't be treated.
Further reading:
1. http://www.nhs.uk/conditions/angiography/Pages/Introduction.aspx
2. http://www.patient.co.uk/health/colonoscopy
3. http://www.nhs.uk/conditions/arthroscopy/pages/introduction.aspx
Sleep studies
This is where patients are checked for problems with oxygen levels in the blood at night during sleep. The most common reason for this is obstructive sleep apnoea, where breathing can pause for a number of seconds during sleep, leading to a decline in blood oxygen levels. This leads to daytime sleepiness and poor concentration. In this test, the patient wears an oxygen monitor, and any 'dips' are recorded. Other parameters can be measured such as heart rate, blood pressure and body movement. If the pattern meets the diagnostic criteria, then a formal diagnosis can be made and suitable treatments tried, such as a positive air pressure machine.
Further reading:
1. http://www.nhs.uk/Conditions/Sleep-apnoea/Pages/diagnosis.aspx
2. http://www.ucmc150.uchicago.edu/sleep/studies.html
So that's my whistle stop tour of the major investigations available to use today! I hope you found it informative.